Q: What common cancer can you prevent with screening?
|
| Colorectal cancer is the number 3 cancer killer in the United States, yet it is one of the most preventable types of cancer. Yes, colorectal cancer can be prevented—not just detected—through colonoscopy. Colorectal cancer arises from pre-cancerous growths or polyps that grow in the colon. When detected early, polyps can be removed, halting their progression to colorectal cancer. While early detection of any cancer is important, prevention is powerful. |
Q: |
What are the risk factors for Colorectal Cancer? |
|
| Lifetime risk of colorectal cancer is 1 in 23 for men and 1 in 25 for women. | ||
| Colorectal cancer is most common after age 50, but it can strike at younger ages. The risk of developing colorectal cancer increases with age. | ||
Q: |
Who is considered High Risk for Colorectal Cancer? |
|
A: |
Colonoscopy is recommended for individuals of any age who are at higher than average risk for developing colorectal cancer by virtue of: |
|
| Personal history of colorectal cancer or colorectal polyps | ||
| A strong family history of the disease | ||
| Inherited forms of colorectal polyps or cancer | ||
| Predisposing chronic digestive condition such as inflammatory bowel disease (Crohn’s disease or ulcerative colitis) | ||
| Recommendations for how often colonoscopy should be performed vary for different subsets of high risk individuals, and they should consult with their physician. | ||
Q: |
What are the symptoms of Colorectal Cancer? |
|
A: |
Most early colorectal cancers produce no symptoms. This is why screening for colorectal cancer is so important. Some possible symptoms, listed below, do not always indicate the presence of colorectal cancer, but should prompt a visit with your physician and a check-up: |
|
| New onset of abdominal pain | ||
| Blood in or on the stool or a change in stool caliber or shape | ||
| A change in typical bowel habits, constipation, diarrhea | ||
Q: |
Why is Colorectal Cancer screening so important? |
|
A: |
Screening tests can find polyps so they can be removed before they turn into cancer. |
|
| Most colorectal cancers develop from polyps, which are abnormal growths in the colon. If polyps grow unnoticed and are not removed, they may become cancerous. Screening tests can find pre-cancerous polyps so they can be removed before they turn into cancer. | ||
| The development of more than 75-90 percent of colorectal cancer can be avoided through early detection and removal of pre-cancerous polyps.* | ||
| * Winawer SJ, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993 Dec 30;329(27):1977-81 | ||
| Learn About Your Screening Options for Colorectal Cancer | ||
| The American College of Gastroenterology 2021 Guidelines on Colorectal Cancer Screening explain the difference between recommended tests that are “one-step tests” and “two-step tests.” In many instances, the best screening test is the one that gets done. | ||
| One-Step Screening Test: Colonoscopy | ||
| Colonoscopy is a one-step test that looks for growths called polyps in your entire colon (large intestine) and rectum using a colonoscope. Your doctor can both detect and remove polyps during colonoscopy and prevent colorectal cancer. Colonoscopy is the most commonly performed gastrointestinal procedure in the United States. Colonoscopy with removal of polyps offers long term protection against developing colorectal cancer or dying from it. | ||
| Two-Step Screening Tests: Stool-Based Tests | ||
| These tests detect blood or altered DNA in the stool as a first step. A positive result would lead to the second step of colonoscopy for further examination. | ||
| FIT Test Fecal Immunochemical Tests (FIT) detects hidden blood in the stool. The stool FIT test is typically performed on an annual basis. A positive test requires a follow-up colonoscopy. |
||
| Multitarget Stool DNA (mtsDNA) Multitarget stool DNA test is a non-invasive screening for colorectal cancer. It looks for abnormal DNA associated with colon cancer or precancerous polyps. This test is more sensitive than the FIT test, but your chance of getting a false positive may increase with advancing age. According to the manufacturer’s recommendations, if the mtsDNA test is negative, repeat screening occurs in three years. If the mtsDNA test is positive, the second step of colonoscopy is required. (At this time the only FDA-approved mtsDNA is Cologuard.®) |
||
| Tests for Individuals who Cannot or Will Not Have a Colonoscopy or FIT, or Are Not Candidates for Colonoscopy | ||
| CT Colonography and Colon Capsule At this time, CT colonography and colon capsule are options for individuals unwilling or unable to undergo colonoscopy or FIT, provided that the tests are locally available and reimbursed by insurers for screening. It is important to note that both tests will still require a follow-up colonoscopy if positive. |
||
| Colorectal Cancer Screening Recommendations | ||
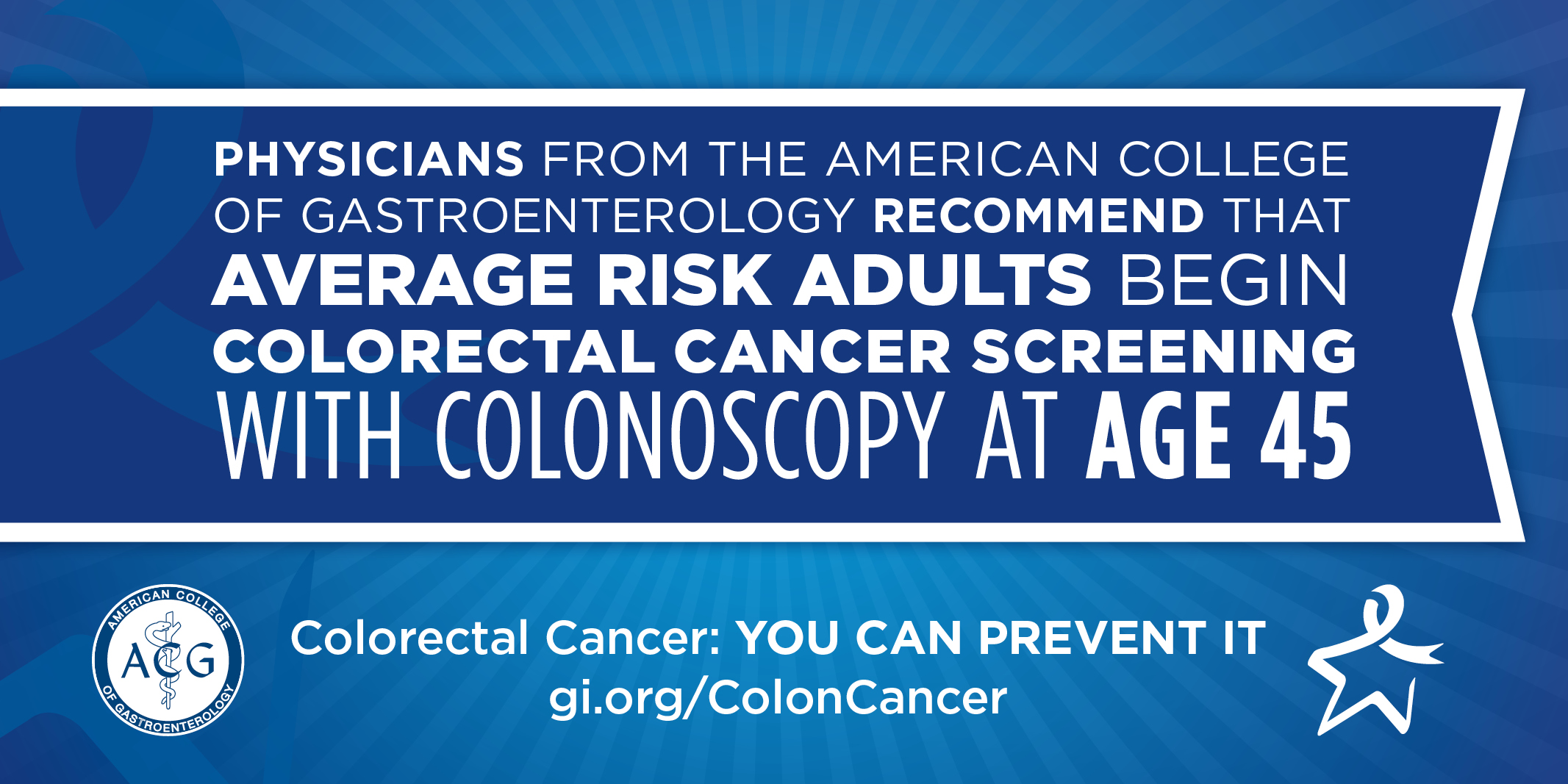
| In 2021, the American College of Gastroenterology updated its colorectal cancer screening guideline. Important recommendations from the authors of guideline are summarized here.* | ||
Recommended Frequency for Different Screening Tests
Screening for Patients with Family History of Colorectal Cancer or Polyps
*Shaukat, et al., American College of Gastroenterology Guideline on Colorectal Cancer Screening, The American Journal of Gastroenterology, March 2021 bit.ly/ACG2021-CRC-Guideline |
||

